Alex Constantine - November 23, 2008
By Ellen Gabler
Milwaukee-Wisconsin Journal Sentinel
Posted: Nov. 22, 2008
Bruce Bowman shouldn't have died the way he did, his children say.
His throat shouldn't have swelled up. His body shouldn't have gone rigid. He shouldn't have gotten pneumonia. The once strong former logger shouldn't have withered away. Two weeks before he died June 19, Bowman weighed 112 pounds.
The 71-year-old man had dementia and was a resident at Taylor Park Nursing and Rehabilitation Center in Rhinelander.
Six months before he died, Bowman started taking Risperdal, an anti-psychotic drug prescribed to control his "agitation" and "physical aggression," according to medical records.
Bowman's children believe the drug killed him.
They insist they were never told by the nursing home staff that Risperdal has a black-box warning that reads: "Increased mortality in elderly patients with dementia-related psychosis."
They didn't know that in clinical trials for Risperdal, most patient deaths occurred from cardiovascular or infectious complications, such as pneumonia. The drug's listed side effects also include vomiting, weight loss and muscle stiffness, among many others.
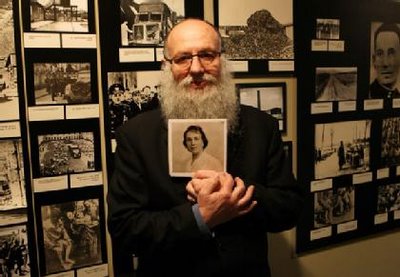
"I'd never give any kind of consent for any of that," said Martin Bowman, Bruce's son, who was the legal guardian of his father's care and needed to approve any changes in medication.
The black-box warning for Risperdal was issued by the Food and Drug Administration in 2005. The drug is approved for use in people with schizophrenia, bipolar disorder and some irritability associated with autism.
But Martin Bowman never saw that warning because the nursing home was using nearly 7-year-old medication consent forms, Public Investigator found.
Before administering a drug to a patient, the nursing home had the patient's legal guardian sign a form that detailed a medication's risks.
But the old forms didn't have the paragraphs of warnings about Risperdal because the warnings hadn't been issued in 2001, when the forms apparently were printed.
A spokesman for Prestige Healthcare, the company that owns Taylor Park nursing home, declined to comment on Bowman's situation, the outdated consent forms or the nursing home's general procedures.
The nursing home could have downloaded an updated form from the state Department of Health Services Web site. But the forms - updated or not - aren't required in nursing homes, according to the department.
A patient, or his or her legal guardian, can be informed verbally about a drug's risks. Martin Bowman said he was not verbally informed about the risks and would never have given permission if he had known.
Bruce Bowman's family said they visited him at least once a week while he was at Taylor Park. They noticed his deterioration - the drooling; his rigid, claw-like hands; his trouble swallowing; and his weight loss - and asked the nurses what was wrong. No one had any answers, said Lisa MaKarrall, Bruce Bowman's daughter. It wasn't until May when Bruce's ex-wife, a former registered nurse, called a hospital psychiatry ward that they found out that Risperdal had a black-box warning, MaKarrall said.
No regulations violated
The state Bureau of Nursing Home Resident Care investigated Taylor Park this summer and again this fall after Bruce Bowman's daughter complained about how her father had been treated. The agency found Taylor Park and its staff did not violate any federal regulations in giving Risperdal to Bruce Bowman.
But his family still wants others to know the dangers of the drug.
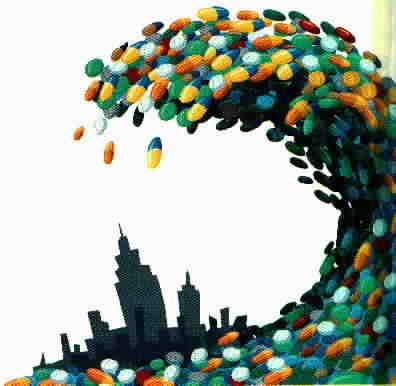
Anti-psychotic drugs often are prescribed to elderly patients with dementia to control their agitation and outbursts. But some of the drugs, such as Risperdal, are not approved for elderly patients with dementia and have the black-box warning.
A handful of states have sued the company that makes and markets Risperdal, Janssen Pharmaceutica of Johnson & Johnson. The states contend the company failed to disclose many of the dangers of the drug. The lawsuits also claim the company marketed the drug to populations for which it had not been approved - such as elderly people. That is against the law.
Janssen spokeswoman Kara Russell said the company denies the allegations.
Many of the states also are suing Janssen to recoup millions of taxpayer dollars spent from Medicaid programs for prescriptions for unapproved uses.
Some researches worry that the anti-psychotic drugs might be overprescribed to subdue nursing-home patients. The consequences can be deadly.
"If someone died from an anti-psychotic, you don't get a second chance," said Thomas E. Lackner, a doctor of pharmacy and professor at the University of Minnesota's College of Pharmacy.
Lackner said using an anti-psychotic drug on elderly patients with dementia is usually a last resort. But sometimes the drugs are helpful, doctors say.
Even though Risperdal and other anti-psychotic drugs aren't approved for treating patients with dementia-related psychosis, that doesn't mean doctors can't prescribe the drugs off-label, or for a purpose other than the drug's approved use.
This practice happens often for all sorts of drugs, doctors say.
"There sometimes aren't any other options," said Edmund H. Duthie, professor of medicine and chief of geriatrics at the Medical College of Wisconsin.
http://www.jsonline.com/watchdog/pi/34942879.html